Radiation is key to the fight against cancer, helping to save countless lives worldwide. But too little radiation can mean ineffective treatment, while too much can cause harm. That’s where dosimetry comes in.
Dosimetry is the science of measuring, calculating and assessing doses of radiation absorbed. It is used by medical physicists to ensure that machines delivering radiation to patients are accurate and properly calibrated. This is critical to patient safety.
So, what goes into dosimetry? How is it kept reliable? To find out more, we sat down with David Followill, Director of Imaging and Radiation Oncology Core (IROC) at Houston Quality Assurance Center at the University of Texas MD Anderson Cancer Center in the United States. IROC Houston is home to the largest dosimetry quality assurance centre in the world, which has assisted 2200 radiotherapy centres in 58 countries. As director of the center and with more than 20 years of experience in dosimetry, Followill has devoted his career to ensuring the accurate, consistent and safe delivery of radiotherapy to cancer patients.
Followill is also one of the invited speakers at the International Symposium on Standards, Applications and Quality Assurance in Medical Radiation Dosimetry (IDOS 2019). The conference begins next week and will provide a forum to discuss advances in the field over the last decade.
Dosimetry is used to keep radiotherapy safe and effective, but how do we ensure dosimetry itself is reliable?
Humans make mistakes. These can be either an individual mistake with one X-ray or electron beam or a systemic mistake that affects all the beams involved in radiation delivery. These kinds of mistakes can go unnoticed unless someone is double-checking the doses. The dosimetry audits we perform at IROC Houston, and those done by the IAEA, as well as other institutions around the world, are vital to ensuring accurate and consistent doses.
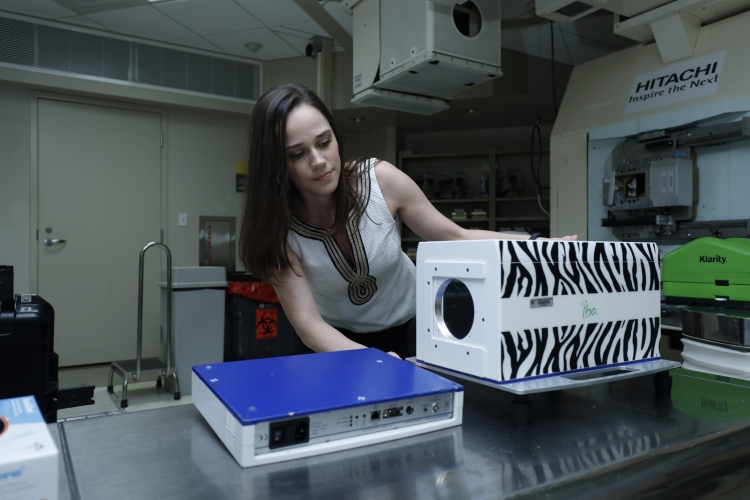
Audits are independent peer-reviews of a clinic’s radiotherapy treatments. Clinics are provided with passive dosimeters (devices designed to measure an absorbed dose of radiation), which the clinic irradiates and sends back to the auditing programme to be evaluated. The audit results confirm if clinics are measuring doses correctly and help them identify and correct any potential mistakes. Getting others to take a second look means they can be confident in the accuracy of their dosimetry measurements.
What do you think is needed to build and maintain a sound dosimetry programme at an institution?
Any clinic’s dosimetry programme needs to start with the robust training of medical physicists. Medical physicists need to not only know how to use the dosimetry equipment but to truly understand how it works to be able to judge if readings are correct or not. They need to always be critical, constantly reviewing their information and be willing to admit if they have made a mistake.
Every clinic also needs reliable equipment that is continually calibrated and subject to quality assurance reviews, so that it produces accurate and consistent readings. With the help of additional educational courses and peer-review papers, health professionals can continue to understand and move past resource limitations. Only in these ways can clinics be sure that the patients are getting as close to the most accurate dose as possible.