Cancer rates are increasing around the world, but most low- and middle-income countries still lack effective services to care for patients. As the number of cancer patients grows, governments are increasingly seeking specialist support to build their capacities to meet their cancer control needs.
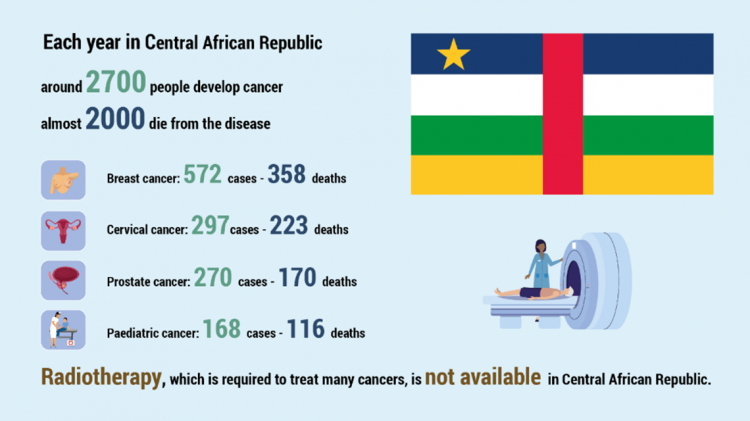
The Central African Republic is no exception. The country has no radiotherapy unit, with access to very limited diagnostic and treatment capacities. Patients and their families who live far from the capital have to travel great distances at considerable expense to reach care. Limited public awareness of cancer symptoms means that many patients seek help only when they have late stage cancers, which are uncurable and only limited end-of-life care can be provided.
A team of nine experts from the IAEA, the World Health Organization (WHO) and the International Agency for Research on Cancer (IARC) recently completed a virtual imPACT Review in the Central African Republic at the request of the Government. They examined the country’s capacities and needs across every stage of cancer control – planning, surveillance, prevention, early detection, diagnosis, treatment and palliative care – and offered a broad range of recommendations which also related to cancer case data collection, specialist training for staff and the development of national cancer control standards and guidelines. The IARC estimates that currently new cancer cases and deaths in the country will rise by almost 30 per cent by 2030.
“The imPACT Review highlighted a number of issues that we must address,” said Raphael Mbailo, Head of Health Directorate at the country’s Ministry of Health and Population. “When we refer cancer patients for treatment outside the country, this can be very costly, and sometimes too late. We want to improve care for cancer patients by supporting consultations with multidisciplinary medical experts, and we need to improve our collection of morbidity and mortality data. Stronger public-private partnerships would help us to work more effectively.”
The Review team paid particular attention to aspects related to breast, cervical and prostate cancers, due to their relatively high prevalence in the country. The team worked with senior medical staff at facilities currently providing cancer services in the capital, Bangui. This included university hospitals, the National Laboratory, the Faculty of Sciences and the National Regulatory Authority for radiation safety. The review also covered relevant aspects of radiation safety and security, with the aim of improving the protection of staff, patients and the environment.
“Our priorities are to increase communication and information about the main cancers and to reinforce the capacity of university hospitals in modern means of cancer diagnosis, training of specialists in medical and surgical oncology and increase the availability of therapeutic services,” said Doui Doumbga, Head of General Surgery Services at Hôpital de l'Amitié in Bangui.