If you would like to learn more about the IAEA’s work, sign up for our weekly updates containing our most important news, multimedia and more.
Combatting Malaria, Dengue and Zika Using Nuclear Technology
Nicole Jawerth

A male Aedes species mosquito. (Photo: IAEA)
Combatting malaria, dengue and Zika using nuclear technology
Diseases such as malaria, dengue and Zika, spread by various mosquito species, are wreaking havoc on millions of lives worldwide. To combat these harmful and often life-threatening diseases, experts in many countries are turning to nuclear and nuclear-derived techniques for both disease detection and insect control.
“ Diagnostic imaging is able to detect malaria infections that have not been detected through routine screenings.
Dengue and Zika
The dengue virus and Zika virus are mainly spread by Aedes species mosquitoes, which are most common in tropical regions. In most cases, the dengue virus causes debilitating flu-like symptoms, but all four strains of the virus also have the potential to cause severe, life-threatening diseases. In the case of the Zika virus, many infected people are asymptomatic or only have mild symptoms; however, the virus can cause serious birth defects in newborns, and it can lead to a debilitating neurological disorder in some adults.
One of the most accurate and widely used laboratory methods for detecting the dengue and Zika viruses is reverse transcription–polymerase chain reaction (RT–PCR). Experts across the world have been trained and equipped by the IAEA to use this technique for detecting, tracking and studying pathogens such as viruses. The diagnostic results help health care professionals to provide treatment and enable experts to track the viruses and take action to control their spread.
When a new outbreak of disease struck in 2015 and 2016, physicians weren’t sure of its cause, but RT–PCR helped to determine that the outbreak was the Zika virus and not another virus such as dengue. RT–PCR was used to detect the virus in infected people throughout the epidemic, which was declared a public health emergency of international concern by the World Health Organization (WHO) in January 2016. During that time, many countries received support from the IAEA, in cooperation with the Food and Agriculture Organization of the United Nations (FAO), in using this method.
While the ongoing Zika threat has been manageable since the epidemic ended in November 2016, dengue has continued to be a growing problem. Some countries in Latin America and the Caribbean, for example, reported increases of up to three times the number of dengue cases in January 2020 compared to the same period in 2019. Meanwhile, in Asia, over 80 000 cases were reported in Bangladesh in 2019, making it the country’s largest dengue outbreak on record.
The situation has been further compounded by the global COVID-19 pandemic that began in early 2020. “The combination of dengue and COVID-19 has overburdened many health care systems,” said Diana Paez, Head of the Nuclear Medicine and Diagnostic Imaging Section at the IAEA. “This is further exacerbated by dengue and COVID-19 sharing similar symptoms and some laboratory features, making differential diagnosis difficult. When one disease is misdiagnosed as the other, it complicates disease management and control, which is why accurate tests like RT–PCR are critical.”
Besides diagnosing and tracking these diseases in people, experts have been looking for ways to reduce the virus-spreading Aedes mosquito population. One option has been area-wide insect management using, among other techniques, a nuclear-based insect birth control method called the sterile insect technique (SIT) (see The Science below).
“SIT has been successfully implemented against numerous insect pests of agricultural importance and is now being adapted for use against mosquitoes,” said Rafael Argilés Herrero, entomologist at the Joint FAO/IAEA Division of Nuclear Techniques in Food and Agriculture. “The method is very specific to the target species and has no impact on other living organisms or the environment.”
Research on the use of SIT against Aedes mosquitoes has intensified worldwide, in part through IAEA and FAO support. Examples include a four-year project launched in 2016 to help countries in the Latin America and the Caribbean region. In 2019, upon Bangladesh’s request, a four-year work plan was agreed for testing SIT for suppressing dengue-spreading mosquitoes. Projects have also been launched in Asia and Europe, and pilot tests have been initiated in 13 countries worldwide, with some achieving as high as 95% suppression.
In early 2020, the IAEA, FAO, Special Programme for Research and Training in Tropical Diseases (TDR) and WHO released the Guidance Framework for Testing the Sterile Insect Technique as a Vector Control Tool against Aedes-Borne Diseases. The publication outlines how an SIT programme can be initiated and how to decide whether to implement it in a country’s affected areas.
Malaria
Malaria is an infectious parasitic disease spread by female Anopheles mosquitoes. This disease threatens approximately half of the world’s population by causing a range of adverse health symptoms and, in some cases, death.
Health professionals can diagnose malaria by testing a patient’s blood for microscopic signs of the parasite, as well as by measuring antigens from the immune system’s response to the parasite. Polymerase chain reaction (PCR) testing is also able to detect malaria, particularly in cases with low levels of parasites or when other infections are present. Through medical imaging techniques such as X-ray and computed tomography (CT), physicians can evaluate the clinical complications of the disease.
“Diagnostic imaging is able to detect malaria infections that have not been detected through routine screenings,” said Hadj Slimane Cherif, Head of the Office of Peaceful Nuclear Technology of Oman’s Ministry of Foreign Affairs. He explained how the number of reported malaria cases has dropped in Oman in the last two decades and the significant role molecular diagnostic imaging methods, acquired through the IAEA’s technical cooperation programme, play in the country’s new policy to screen travellers from malaria-endemic places. “This policy will eventually lead to Oman becoming a malaria-free country.”
By reducing the population of Anopheles mosquitoes using SIT, experts are also hoping to reduce the spread of malaria. Some technical challenges they face have been ensuring only male sterilized mosquitoes are released, as well as developing efficient trapping systems. This has created obstacles to the large-scale use of SIT against this type of mosquito.
One of the ongoing challenges with SIT for mosquito control is how to effectively release these fragile insects. In June 2020, researchers found that using drones to release sterilized males was more cost-effective, faster and less damaging to the mosquitoes than other common release methods, such as on-the-ground or by airplane. These findings marked a major breakthrough in expanding the use of SIT against mosquitoes.
THE SCIENCE
Sterile Insect Technique
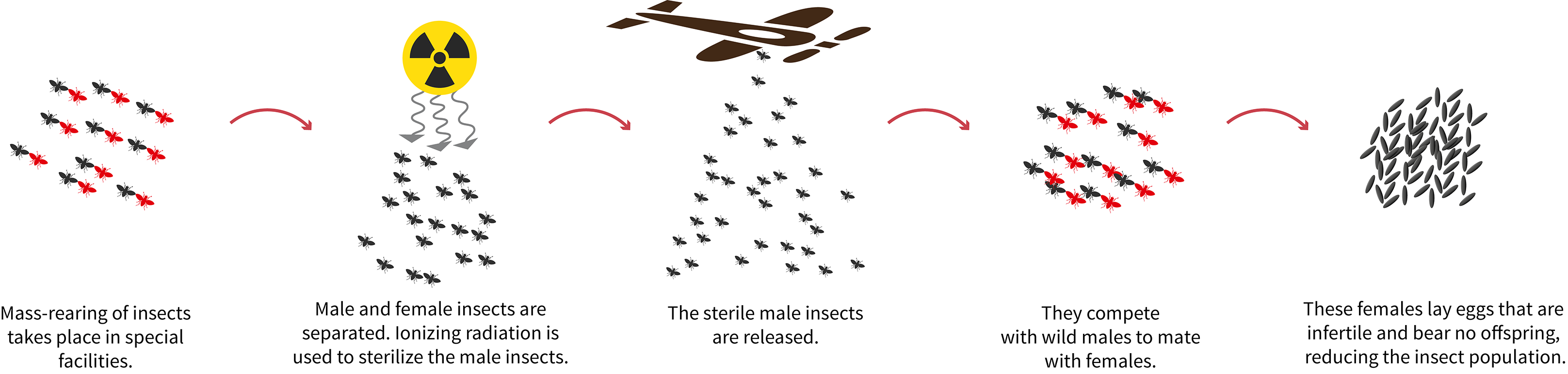
The sterile insect technique (SIT) uses radiation to sterilize male insects that are mass produced in special facilities. Large quantities of the sterile male insects are systematically released from the ground or by air. They mate with wild females in nature, which results in no new offspring. Over time, this brings the insect population down, or, when insect populations are isolated, it can eradicate an entire population. SIT has been successfully used for over 50 years against agricultural insect pests.